“It’s Time To Talk About Prostate Cancer
By Rodney Folmar, Sr.
Even though prostate cancer has a high survival rate when compared to other forms of cancer, approximately a quarter of a million people are diagnosed with prostate cancer every year and between 30,000 and 40,000 men die from prostate cancer annually.
According to the American Cancer Society, prostate cancer is the most common cause of new cancer in men, responsible for more than 20 percent of new cancer cases in men. Prostate cancer is also responsiblefor ten percent of all male deaths due to cancer annually, ranking it second (behind lung cancer).
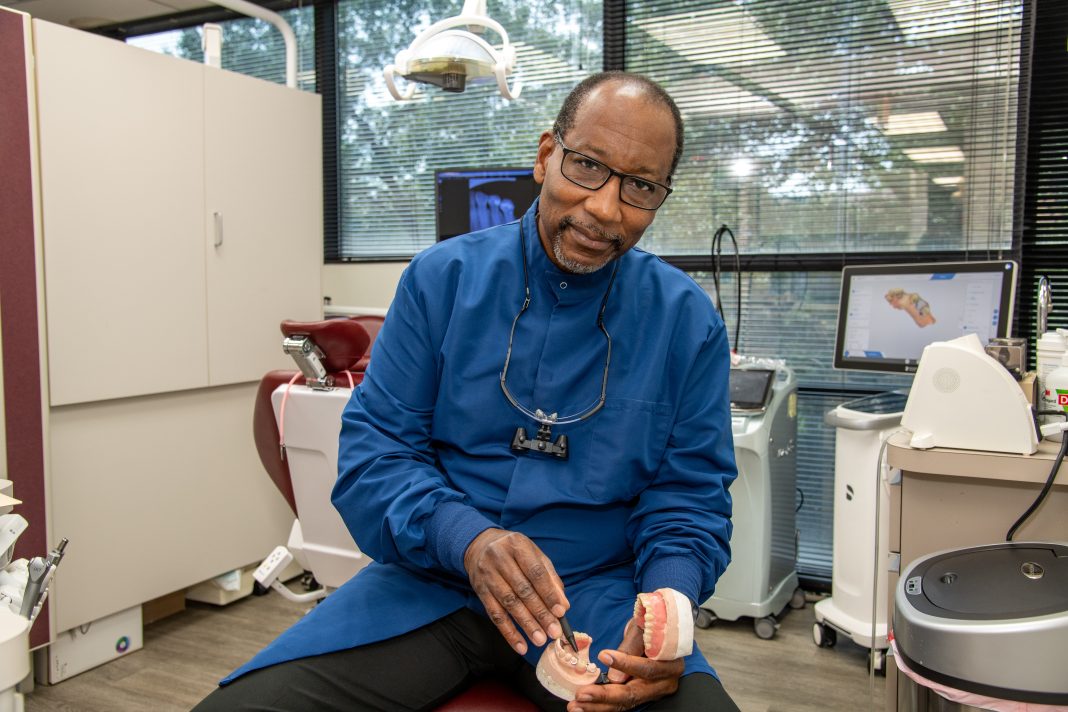
We sat down with one of the country’s leading urologists, Dr. Mutahar Ahmed, to discuss the current recommendations, diagnosis, and treatment process in prostate cancer.
Dr. Ahmed was born in Bangladesh but emigrated to the United States at an early age. He grew up in Manhattan and the Bronx, attending New York City public schools. He graduated from New York University before completing medical school at SUNY Syracuse Medical School.
He completed his General Surgery and Urology residency at Rutgers University Medical School in 2003 and went into private practice with New Jersey Urology. Since he joined the practice, it has expanded and is now the largest Urology practice in the country.
| DIAGNOSIS
The key to effectively diagnosing and treating prostate cancer is adequate testing. Right now, the recommendation is that all men should get tested for prostate cancer either annually or biannually (every other year) starting at age 50. Individuals with risk factors that make them more likely to develop prostate cancer should start testing at a younger age.
Examples of risk factors for prostate cancer include:
African – American ancestry
Obesity
High-fat diet
Older age
A close family member with prostate cancer
The initial test for prostate cancer is a blood test called PSA (prostate-specific antigen). In the past, an elevated PSA (greater than 4.0 ng/mL) would lead to an immediate biopsy. Now, Dr. Ahmed says this is no longer the case. Even though a biopsy is a great way to diagnose prostate cancer, it is invasive, and not everyone with an elevated PSA necessarily has prostate cancer. The PSA blood test is combined with a digital rectal exam (DRE) to screen for prostate cancer regularly.
SCREENING
Instead, Dr. Ahmed and the American Urological Association (AUA) recommend that individuals with an elevated PSA get a screening MRI first, which most insurance companies should cover. There are numerous benefits of getting a screening MRI following an elevated PSA, including:
• If the MRI is clean, it could spare someone from an invasive biopsy
• If the MRI is abnormal, it gives the urologist a target to hit on the biopsy
• It can prevent a lot of emotional, mental, and physical stress by saving people from cancer treatment that is unnecessary.
• If a biopsy is required, the pathologist will stratify patients into a specific prostate cancer group using something called a Gleason score.
The Gleason score is a combination of two numbers added together and can range from 2
(1+1) to 10 (5+5). A Gleason score of 6 or higher places patients into a prostate cancer group:
•Group 1, Gleason Score 6 (3+3): This is a low-risk group with a very favorable result that requires active surveillance.
• Group 2, Gleason Score 7 (3+4): This is an intermediate group with favorable results. Patients in this category with a relatively clean biopsy, MRI, and digital rectal exam with a low PSA score might undergo active surveillance; however, if the biopsy showed several cores of prostate cancer with an elevated percentage of positive cells in each core, this group might get treated.
•Group 3, Gleason Score 7 (4+3): This is an intermediate group with unfavorable results and requires treatment.
•Group 4, Gleason Score 8 (4+4): High-risk group that requires treatment.
•Group 5, Gleason Score 9 or 10 (4+5, 5+4, 5+5): This is a very high group that requires treatment.
What is active surveillance? Patients undergoing active surveillance need to follow up with their doctor more often. They need a repeat PSA screen in 3 to 4 months with another biopsy in one year. If the results on the biopsy are unchanged, then the patient can return to the normal prostate cancer screening schedule.
|SURGERY
If a patient requires treatment for prostate cancer, there are two broad options. The first is surgery. Surgery is usually recommended for younger individuals. Most prostate cancer resections are now performed laparoscopically. A laparoscopic surgical procedure is performed using a handful of small incisions (5 to 6 incisions only a cm or two in size) instead of a larger incision. This expedites the recovery process.
In New Jersey, Dr. Ahmed is one of two surgeons who can perform prostate cancer resection using a single incision at the back of the body instead of the front, sparing multiple incisions and reducing the risk of damaging the abdominal organs. Even though this new surgical approach was developed well into Dr. Ahmed’s career, he decided to learn this new approach because he believes it is better for his patients and their qualities of life. For example, patients can usually go home the same day as the procedure is performed, shortening the recovery process.
|POSSIBLE SIDE EFFECTS
There are a few possible complications of prostate cancer surgery. Even though every attempt is made to spare the pudendal nerve, patients may have difficulty maintaining an erection for a few weeks following this procedure. Patients also have to go home with a catheter for a short period of time. Most side effects and complications of prostate cancer surgery fade with time.
The other treatment option is radiation therapy, which is recommended for older individuals or those with prostate cancer that has spread outside of a localized area. There are multiple types of radiation therapy, which will be discussed in detail with each patient before a decision is made.
While radiation therapy might not have as many immediate complications and side effects, the cumulative effects of radiation can add up over time. Patients can develop urinary and reproductive difficulties as a result of radiation. A major concern with using radiation therapy in younger patients is that they could develop secondary cancers as a result. While radiation therapy is targeted to cancerous cells, some healthy cells are going to be harmed in the process. Even though these healthy cells will not become cancerous immediately, some types of cancer could develop decades down the road.
Every patient will discuss the benefits and drawbacks of surgery and radiation with their doctor if prostate cancer treatment is required. Surgery is usually recommended in younger patients while radiation therapy is typically recommended in older patients.
Finally, Dr. Ahmed wants all men to remember, prostate cancer is not a death sentence; however, it can be a death sentence if you don’t know what you have. Therefore, all men should get tested regularly in accordance with the guidelines above. The earlier prostate cancer is detected, the better the prognosis, and not everyone who has been diagnosed with prostate cancer needs to be treated.
To learn more about prostate cancer, visit the Prostate Cancer Foundation and the American Urological Association, or consult the list of local Urologist.
TOP UROLOGIST IN MD, DC & VA
Medstar Georgetown Cancer Institute
MedStar Southern Maryland Hospital Center
7503 Surratts Road
Clinton, MD 20735
Dr. Christen A. Alevizatos, MD
Chief of Urology
Good Samaritan Hospital
6535 N. Charles Street
Suite 500
Townson, MD 21204
Johns Hopkins Health Care & Surgery Center
10803 Falls Road
Pavilion III
Suite 3300
Lutherville, MD 21093
Surgery Center in National Harbor
251 National Harbor Blvd.
Suite 400-A
National Harbor, MD 20745
*5 Locations VA & MD
Urology Specialist of Maryland
301 St. Paul Place
Baltimore, MD
810 Bestgate Road
Suite 235
Annapolis, MD 21401
*Multiple Locations
400 West 7th Street
Frederick, MD 21701
AA Urology
4201 Northview Drive
Suite 201
Bowie, MD 20716
Family Urology Associates
186 Thomas Johnson Drive
Suite 104
Frederick, MD 21702
Urology Consultants of Maryland
77 Thomas Johnson Drive
Suite K
Frederick, MD 21702
University of Maryland Surgical Associates
419 West Redwood Street
Suite 310
Baltimore, MD 21201
Urologic Surgeons of Washington
1147 20th Street NW
Suite 400
Washington, DC 20036